*Drs. Yifan Zhai and Xiaojun Huang are co-corresponding authors.
Introduction
This was a multicenter, randomized, registrational phase 2 study to assess the efficacy and safety of olverembatinib compared with BAT in pts with CML-CP who were resistant and/or intolerant to 3 TKIs (imatinib [I], dasatinib [D], nilotinib [N]) in China.
Methods
Eligible adult CML-CP pts were resistant and/or intolerant to 3 TKIs, were in ECOG PS 0-2, and had adequate organ function. Pts were randomized 2:1 to investigational olverembatinib (40 mg QOD) or the BAT arm, which could be one of the following per investigator choice: TKIs (I, D, or N), interferon (IFN), hydroxyurea (HU), and homoharringtonine (HHT). The primary endpoint was event-free survival (EFS), including time from randomization to AP or BP progression); all-cause mortality; relapse; treatment failure (no complete remission [CR] within 3 cycles); loss of complete hematologic response (CHR); and treatment intolerance as per investigator and study sponsor. Efficacy was analyzed in the intention-to-treat (ITT) efficacy population and safety in pts receiving ≥1 dose of olverembatinib.
Results
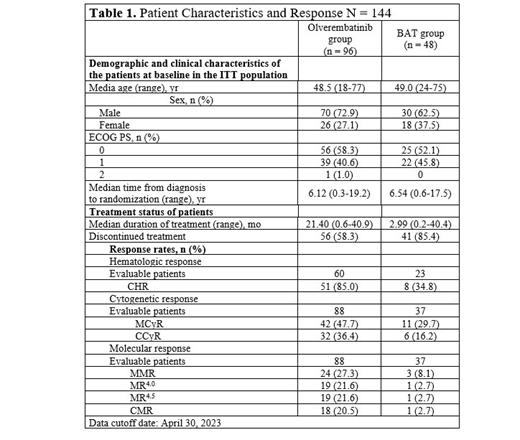
As of April 30, 2023, a total of 144 pts (96, olverembatinib; 48, BAT) were enrolled, including 69.4% male and 30.6% female, with a median (range) age of 49.0 (18-77) years. A total of 129 pts (89.6%) were previously treated with ≥ 3 TKIs (I, D, N). 15 pts (10.5%) with T315I mutation received ≥1 TKIs, of whom 9 (6.3%) received 2. Median (range) follow-up was 12.67 (0.0-40.9) and 2.94 (0.0-40.4) months in the olverembatinib and BAT arms, respectively. A total of 66 (45.8%) pts had ≥1 BCR::ABL1 mutation and 39 (27.1%) BCR::ABL1 T315I. A total of 97 pts discontinued therapies (56 [58.3%] olverembatinib, 41 [85.4%] BAT) due to disease progression/treatment failure, AE, consent withdrawal, poor compliance, or death. In the safety population, 82/96 (85.4%) pts receiving olverembatinib and 31/46 (67.4%) BAT experienced a grade ≥ 3 AE. Any-grade AEs (> 20% incidence) included thrombocytopenia; leukopenia; anemia; neutropenia; elevated CPK, ALT, and AST; and hypertriglyceridemia. Serious AEs (SAEs) (>5%) included thrombocytopenia. A total of 7 SAEs were possibly related to olverembatinib: 1 acute myocardial infarction, 3 coronary heart disease cases, 2 cerebral infarctions, and 1 congestive heart failure. Common AEs (≥10%) leading to discontinuation, dose reduction, or treatment withdrawal were thrombocytopenia, neutropenia, and leukopenia.
Median (range) EFS was 21.22 (95% CI, 10.15-NR) months in the olverembatinib arm and 2.86 (95% CI 2.53-4.73) months in the BAT arm ( P < .001; HR, 0.352; 95% CI, 0.228-0.545). Compared with the BAT control arm, olverembatinib reduced the event risk 65%. In the olverembatinib arm, estimated EFS at 6, 12, and 24 months was 73% (95% CI, 62.5-81.0), 58.7% (95% CI, 47.5-68.2), and 46.9% (95% CI, 35.9-57.2), respectively. In the BAT group, it was 32.6% (95% CI, 19.7-46.2), 26.1% (95% CI, 14.5-39.3), and 16.9% (95% CI, 7.7-29.2), respectively. Median OS was NR in either group ( P = .41). Up to data cutoff, 34 (71%) pts in the BAT control arm were crossed-over to be treated with olverembatinib after EFS endpoint was reached. In the ITT efficacy group, among those treated with olverembatinib, 51/60 (85%) pts achieved a CHR; 42/88 (47.7%) MCyR; 32/88 (36.4%) CCyR; and 24/88 (27.3%) MMR. In the BAT group, 8/23 (34.8%) pts achieved a CR, 11/37 (29.7%) MCyR, 6/37 (16.2%) CCyR, and 3/37 (8.1%) MMR.
Conclusions
This study represents the largest population of pts with CML-CP resistant or intolerant to both 1G and 2G TKIs. Olverembatinib was observed to be better tolerated and more effective than BAT in treating these pts. Internal study (CT.gov) numbers: HQP1351CC203 (NCT04126681).
Disclosures
Chen:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Niu:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Men:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Yang:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company, Membership on an entity's Board of Directors or advisory committees, Other: Leadership, Patents & Royalties. Zhai:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company, Other: Leadership (CMO).

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal